America a Narrative History 10th Edition Chapter 20 Quizlet
Main Body
Chapter 19. Health and Medicine
Learning Objectives
19.1. The Social Construction of Health
- Define the term medical sociology
- Understand the difference between the cultural meaning of illness, the social construction of illness, and the social construction of medical knowledge
19.2. Global Health
- Define social epidemiology
- Apply theories of social epidemiology to an understanding of global health issues
- Understand the differences between high-income and low-income nations
19.3. Health in Canada
- Understand how social epidemiology can be applied to health in Canada
- Explain disparities of health based on gender, socioeconomic status, race, and ethnicity
- Give an overview of mental health and disability issues in Canada
- Explain the terms stigma and medicalization
19.4. Theoretical Perspectives on Health and Medicine
- Apply functionalist, conflict theorist, and interactionist perspectives to health issues
Introduction to Health and Medicine
In 2012, a pertussis (whooping cough) outbreak in B.C., Alberta, Ontario, and New Brunswick sickened 2,000 people and resulted in an infant death in Lethbridge. In the United States, where there were 18,000 cases and nine deaths, it was the worst outbreak in 65 years (Picard 2012). Researchers, suspecting that the primary cause of the outbreak was the waning strength of pertussis vaccines in older children, recommended a booster vaccination for 11–12-year-olds and pregnant women (Zacharyczuk 2011). Pertussis is most serious for babies; one in five must be hospitalized, and since they are too young for the vaccine themselves, it is crucial that people around them be immunized (Centers for Disease Control 2011). In response to the outbreak, health authorities in various parts of Canada offered free vaccination clinics for parents with infants under one. Typically Canadian children are vaccinated for whooping cough, diphtheria, and tetanus (a combined vaccine known as DTaP) at ages 2, 4, 6, and 18 months, and then again at ages 4 to 6 years and 14 to 16 years (Picard 2012).
But what of people who do not want their children to have this vaccine, or any other? That question is at the heart of a debate that has been simmering for years. Vaccines are biological preparations that improve immunity against a certain disease. Vaccines have contributed to the eradication and weakening of numerous infectious diseases, including smallpox, polio, mumps, chicken pox, and meningitis.
However, many people express concern about potential negative side effects from vaccines. These concerns range from fears about overloading the child's immune system to controversial reports about devastating side effects of the vaccines. One misapprehension is that the vaccine itself might cause the disease it is supposed to be immunizing against. Another commonly circulated concern is that vaccinations, specifically the MMR vaccine (MMR stands for measles, mumps, and rubella), are linked to autism. The autism connection has been particularly controversial. In 1998, a British physician named Andrew Wakefield published a study in Great Britain's Lancet magazine that linked the MMR vaccine to autism. The report received a lot of media attention, resulting in British immunization rates decreasing from 91 percent in 1997 to almost 80 percent by 2003, accompanied by a subsequent rise in measles cases (Devlin 2008). A prolonged investigation by the British Medical Journal proved that not only was the link in the study nonexistent, but that Dr. Wakefield had falsified data in order to support his claims (CNN 2011). Dr. Wakefield was discredited and stripped of his license, but the doubt still lingers in many parents' minds.
In Canada, many parents still believe in the now-discredited MMR-autism link and refuse to vaccinate their children. Other parents choose not to vaccinate for various reasons like religious or health beliefs. In the United States, a boy whose parents opted not to vaccinate returned home after a trip abroad; no one yet knew he was infected with measles. The boy exposed 839 people to the disease and caused 11 additional cases of measles, all in other unvaccinated children, including one infant who had to be hospitalized. According to a study published in Pediatrics , the outbreak cost the public sector $10,376 per diagnosed case. The study further showed that the intentional non-vaccination of those infected occurred in students from private schools, public charter schools, and public schools in upper-socioeconomic areas (Sugerman et al. 2010).
Should parents be forced to immunize their children? What might sociologists make of the fact that most of the families who chose not to vaccinate were of a higher socioeconomic group? How does this story of vaccines in a high-income region compare to that in a low-income region, like sub-Saharan Africa, where populations are often eagerly seeking vaccines rather than refusing them?
The sociology of health encompasses social epidemiology, disease, mental health, disability, and medicalization. The principle insight of sociology is that health and illness cannot be simply regarded as biological or medical phenomena. They are perceived, organized, and acted on in a political, economic, cultural, and institutional context. Moreover, the way that we relate to them is in constant evolution. As we learn to control existing diseases, new diseases develop. As our society evolves to be more global, the way that diseases spread evolves with it.
According to the World Health Organization (WHO), health "is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity" (WHO 2014). What does "health" mean to you? How does the WHO definition relate to contemporary issues of health? Do you believe that there are too many people taking medications in Canadian society? Are you skeptical about people claiming they are "addicted" to gambling or "addicted" to sex? Can you think of anything that was historically considered a disease, but is now considered within a range of normality? Or anything that has recently become known as a disease, whereas before it was considered evidence of laziness or other character flaws? Do you believe all children should receive vaccinations? These are questions examined in the sociology of health.
Sociologists may also understand these issues more fully by considering them through one of the main theoretical perspectives of the discipline. The functionalist perspective is a macroanalytical perspective that looks at the big picture, focusing on the way that all aspects of society are integral to the continued health and viability of the whole. For those working within the functionalist perspective, the focus is on how healthy individuals have the most to contribute to the stability of society. Functionalists might study the most efficient way to restore "sick" individuals to a healthy state. The critical perspective is another macroanalytical perspective that focuses on the creation and reproduction of inequality. Someone applying the critical perspective might focus on the relationship between the power of pharmaceutical companies and rates of drug prescription, or between medical knowledge and the way power is exercised through the increased medicalization of the body. Someone applying the interactionist perspective to health might focus on how people understand their health, how their relationship to their bodies is mediated by social concepts of health and illness, and how their health affects their relationships with the people in their lives.
19.1 The Social Construction of Health
If sociology is the systematic study of human behaviour in society, medical sociology is the systematic study of how humans manage issues of health and illness, disease and disorders, and health care for both the sick and the healthy. Medical sociologists study the physical, mental, and social components of health and illness. Major topics for medical sociologists include the doctor-patient relationship, the structure and socioeconomics of health care, and how culture impacts attitudes toward disease and wellness.
The social construction of health is a major research topic within medical sociology. At first glance, the concept of a social construction of health does not seem to make sense. After all, if disease is a measurable, physiological problem, then there can be no question of socially constructing disease, right? Well, it's not that simple. The idea of the social construction of health emphasizes the socio-cultural aspects of the discipline's approach to physical, objectively definable phenomena. Sociologists Conrad and Barker (2010) offer a comprehensive framework for understanding the major findings of the last 50 years of development in this concept. Their summary categorizes the findings in the field under three subheadings: the cultural meaning of illness, the social construction of the illness experience, and the social construction of medical knowledge.
The Cultural Meaning of Illness
Many medical sociologists contend that illnesses have both a biological and an experiential component, and that these components exist independently of each other. Our culture, not our biology, dictates which illnesses are stigmatized and which are not, which are considered disabilities and which are not, and which are deemed contestable (meaning some medical professionals may find the existence of this ailment questionable) as opposed to definitive (illnesses that are unquestionably recognized in the medical profession) (Conrad and Barker 2010).
For instance, sociologist Erving Goffman (1963) described how social stigmas hinder individuals from fully integrating into society. The stigmatization of illness often has the greatest effect on the patient and the kind of care he or she receives. Many contend that our society and even our health care institutions discriminate against certain diseases—like mental disorders, AIDS, venereal diseases, and skin disorders (Sartorius 2007). Facilities for these diseases may be sub-par; they may be segregated from other health care areas or relegated to a poorer environment. The stigma may keep people from seeking help for their illness, making it worse than it needs to be.
Contested illnesses are those that are questioned or questionable by some medical professionals. Disorders like fibromyalgia or chronic fatigue syndrome may be either true illnesses or only in the patients' heads, depending on the opinion of the medical professional. This dynamic can affect how a patient seeks treatment and what kind of treatment he or she receives.
The Social Construction of the Illness Experience
The idea of the social construction of the illness experience is based on the concept of reality as a social construction. In other words, there is no objective reality independent of our own perceptions of it. The social construction of the illness experience deals with such issues as the way some patients control the manner in which they reveal their disease and the lifestyle adaptations patients develop to cope with their illnesses.
In terms of constructing the illness experience, culture and individual personality both play a significant role. For some people, a long-term illness can have the effect of making their world smaller, more defined by the illness than anything else. For others, illness can be a chance for discovery, for re-imaging a new self (Conrad and Barker 2010). Culture plays a huge role in how an individual experiences illness. Widespread diseases like AIDS or breast cancer have specific cultural markers that have changed over the years and that govern how individuals—and society—view them.
Today, many institutions of wellness acknowledge the degree to which individual perceptions shape the nature of health and illness. Regarding physical activity, for instance, the Public Health Agency of Canada recommends that individuals use a standard level of exertion to assess their physical activity. This rating of perceived exertion (RPE) gives a more complete view of an individual's actual exertion level, since heart rate or pulse measurements may be affected by medication or other issues (CSEP N.d.). Similarly, many medical professionals use a comparable scale for perceived pain to help determine pain management strategies.
The Social Construction of Medical Knowledge
Conrad and Barker show how medical knowledge is socially constructed; that is, it can both reflect and reproduce inequalities in gender, class, race, and ethnicity. Conrad and Barker (2010) use the example of the social construction of women's health and how medical knowledge has changed significantly in the course of a few generations. For instance, in the early 20th century, pregnant women were discouraged from driving or dancing for fear of harming the unborn child, much as they are discouraged from smoking or drinking alcohol today.
Making Connections: Social Policy & Debate
Has Breast Cancer Awareness Gone Too Far?
Every October, the world turns pink. Football and baseball players wear pink accessories. Skyscrapers and large public buildings are lit with pink lights at night. From retailers, shoppers can choose from a huge array of pink products. In 2011, people wanting to support the fight against breast cancer could purchase any of the following pink products: KitchenAid mixers, Master Lock padlocks and bike chains, Wilson tennis rackets, Fiat cars, and Smith & Wesson handguns. You read that correctly. The goal of all these pink products is to raise awareness and money for breast cancer. However, the relentless creep of pink has many people wondering if the pink marketing juggernaut has gone too far.
Pink has been associated with breast cancer since 1991, when the Susan G. Komen Foundation handed out pink ribbons at its 1991 Race for the Cure event. Since then, the pink ribbon has appeared on countless products, and then by extension, the colour pink has come to represent support for a cure of the disease. No one can argue about the Susan G. Komen Foundation's mission—find a cure for breast cancer—or the fact that the group has raised millions of dollars for research and care. However, some people question if, or how much, all these products really help in the fight against breast cancer (Begos 2011).
The advocacy group Breast Cancer Action (BCA) position themselves as watchdogs of other agencies fighting breast cancer. They accept no funding from entities, like those in the pharmaceutical industry, with potential profit connections to this health industry. They have developed a trademarked "Think Before You Pink" campaign to provoke consumer questioning of the end contributions made to breast cancer by companies hawking pink wares. They do not advise against "pink" purchases; they just want consumers to be informed about how much money is involved, where it comes from, and where it will go. For instance, what percentage of each purchase goes to breast cancer causes? BCA does not judge how much is enough, but it informs customers and then encourages them to consider whether they feel the amount is enough (Think Before You Pink 2012).
BCA also suggests that consumers make sure that the product they are buying does not actually contribute to breast cancer, a phenomenon they call "pinkwashing." This issue made national headlines in 2010, when the Susan G. Komen Foundation partnered with Kentucky Fried Chicken (KFC) on a promotion called "Buckets for the Cure." For every bucket of grilled or regular fried chicken, KFC would donate 50 cents to the Komen Foundation, with the goal of reaching $8 million: the largest single donation received by the foundation. However, some critics saw the partnership as an unholy alliance. Higher body fat and eating fatty foods has been linked to increased cancer risks, and detractors, including BCA, called the Komen Foundation out on this apparent contradiction of goals. Komen's response was that the program did a great deal to raise awareness in low-income communities, where Komen previously had little outreach (Hutchison 2010).
What do you think? Are fundraising and awareness important enough to trump issues of health? What other examples of "pinkwashing" can you think of?
19.2. Global Health
Social epidemiology is the study of the causes and distribution of diseases. Social epidemiology can reveal how social problems are connected to the health of different populations. These epidemiological studies show that the health problems of high-income nations differ greatly from those of low-income nations. Some diseases, like cancer, are universal. But others, like obesity, heart disease, respiratory disease, and diabetes are much more common in high-income countries, and are a direct result of a sedentary lifestyle combined with poor diet. High-income nations also have a higher incidence of depression (Bromet et al. 2011). In contrast, low-income nations suffer significantly from malaria and tuberculosis.
How does health differ around the world? Some theorists differentiate among three types of countries: core nations, semi-peripheral nations, and peripheral nations. Core nations are those that we think of as highly developed or industrialized, semi-peripheral nations are those that are often called developing or newly industrialized, and peripheral nations are those that are relatively undeveloped. While the most pervasive issue in the Canadian care system is timely access to health care, other core countries have different issues, and semi-peripheral and peripheral nations are faced with a host of additional concerns. Reviewing the status of global health offers insight into the various ways that politics and wealth shape access to health care, and it shows which populations are most affected by health disparities.
Health in High-Income Nations
Obesity, which is on the rise in high-income nations, has been linked to many diseases, including cardiovascular problems, musculoskeletal problems, diabetes, and respiratory issues. According to the Organisation for Economic Co-operation and Development (2013), obesity rates are rising in all countries, with the greatest gains being made in the highest-income countries. The United States has the highest obesity rate for adults, while Canada rated fifth. Wallace Huffman and his fellow researchers (2006) contend that several factors are contributing to the rise in obesity in developed countries:
- Improvements in technology and reduced family size have led to a reduction of work to be done in household production.
- Unhealthy market goods, including processed foods, sweetened drinks, and sweet and salty snacks are replacing home-produced goods.
- Leisure activities are growing more sedentary; for example, computer games, web surfing, and television viewing.
- More workers are shifting from active work (agriculture and manufacturing) to service industries.
- Increased access to passive transportation has led to more driving and less walking.
Obesity and weight issues have significant societal costs, including lower life expectancies and higher shared health care costs. High-income countries also have higher rates of depression than less affluent nations. A recent study (Bromet et al. 2011) shows that the average lifetime prevalence of major depressive episodes in the 10 highest-income countries in the study was 14.6 percent; this compared to 11.1 percent in the eight low- and middle-income countries. The researchers speculate that the higher rate of depression may be linked to the greater income inequality that exists in the highest-income nations.
Health in Low-Income Nations
In peripheral nations with low per capita income, it is not the cost of health care that is the most pressing concern. Rather, low-income countries must manage such problems as infectious disease, high infant mortality rates, scarce medical personnel, and inadequate water and sewer systems. Such issues, which high-income countries rarely even think about, are central to the lives of most people in low-income nations. Due to such health concerns, low-income nations have higher rates of infant mortality and lower average life spans.
One of the biggest contributors to medical issues in low-income countries is the lack of access to clean water and basic sanitation resources. According to a 2011 UNICEF report, almost half of the developing world's population lacks improved sanitation facilities. The World Health Organization (WHO) tracks health-related data for 193 countries. In their 2011 World Health Statistics report, they document the following statistics:
- Globally, the rate of mortality for children under five was 60 per 1,000 live births. In low-income countries, however, that rate is almost double at 117 per 1,000 live births. In high-income countries, that rate is significantly lower than 7 per 1,000 live births.
- The most frequent causes of death for children under five were pneumonia and diarrheal diseases, accounting for 18 percent and 15 percent, respectively. These deaths could easily be avoidable with cleaner water and more coverage of available medical care.
- The availability of doctors and nurses in low-income countries is one-tenth that of nations with a high income. Challenges in access to medical education and access to patients exacerbate this issue for would-be medical professionals in low-income countries (World Health Organization 2011).
19.3. Health in Canada
Health in Canada is a complex and often contradictory issue. One the one hand, as one of the wealthiest nations, Canada fares well in health outcomes with respect to the rest of the world. However, while the publicly funded health care system in Canada compares well to the noted issues of the private for-profit system in the United States (especially in terms of overall cost and who gets access to medical care), it is also behind many European countries in terms of key health care indicators such as access to family doctors and wait times for critical procedures. The following sections look at different social aspects of health in Canada.
Health by Race and Ethnicity
Unlike the United States, where strong health disparities exist along racial lines, in Canada differences in health between non-aboriginal visible minorities and Canadians of European origin disappear once socioeconomic status and lifestyle are taken into account. Moreover, new and recent immigrants from non-European countries tend, in fact, to have better health than the average native-born Canadian (Kobayashi, Prus, and Lin 2008).
Aboriginal Canadians unfortunately continue to suffer from serious health problems. It is estimated that in the 1500s, prior to contact, there were 500,000 aboriginal people living in Canada. Through epidemics of contagious Euro-Asian diseases such as smallpox, measles, influenza, and tuberculosis, aboriginal populations suffered an estimated 93 percent decline (O'Donnell 2008). Conditions in the late 19th century to the mid 20th century did not improve markedly after aboriginal people were moved to reserves. Often lacking adequate drinking water, sanitation facilities, and hygienic conditions, these were ideal settings for the spread of communicable diseases. Death rates from tuberculosis (TB), for example, remained very high for First Nations peoples into the 1950s, long after the use of antibiotics brought TB under control in the rest of Canada. In 2005, the TB rate was still 27 active cases per 100,000 population for aboriginal people, while it was only 5 active cases per 100, 000 for the rest of the population. Part of the problem is that the percentage of aboriginal people living in overcrowded housing on reserves and in the north is five to six times higher than for the general population (Statistics Canada 2011). Recent crises in Attawapiskat, Ontario, and other First Nations communities with respect to housing, drinking water, and lack of proper water purification systems indicate that these issues have not been resolved (Stastna 2011).
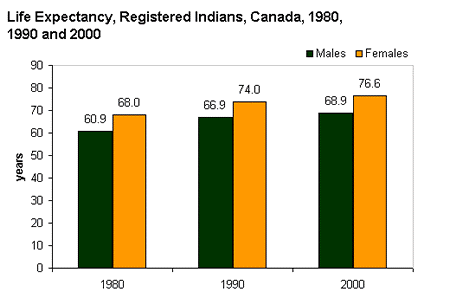
Figure 19.5 shows that life expectancy for aboriginal people (registered Indians) has improved. However, it remains significantly lower than for the average population: Aboriginal men and women could expect to live 8.1 and 5.5 fewer years respectively than the average Canadian man and woman (Health Canada 2005). While infectious diseases are largely regarded now as being under control in aboriginal populations (albeit at higher rates than the Canadian population), aboriginal people suffer disproportionately from chronic health problems like diabetes, heart disease, obesity, respiratory problems, and HIV (Statistics Canada 2011). The health conditions of off-reserve aboriginal people are also significantly worse than for the average population. While nearly 59 percent of non-aboriginal people in Canada over the age of 20 rated their health as "excellent or very good" in 2006–2007, only 51 percent of First Nations, 57 percent of Métis, and 49 percent of Inuit living off-reserve did so. Similarly 74 percent of non-aboriginal Canadians reported that they had no physical limitations due to ill health, while only 58, 59, and 64 percent of off-reserve First Nations, Métis, and Inuit, respectively, did so (Garner, Carrière, and Sanmartin 2010). While some of the difference between aboriginal and non-aboriginal health conditions can be explained by financial, educational, and individual lifestyle variables, even when these were taken into account statistically disparities in health remained. The authors of the study on off-reserve aboriginal health report that "[s]uch findings point to the existence of other factors contributing to the greater burden of morbidity among First Nations, Métis and Inuit people" (Garner, Carrière, and Sanmartin 2010, p. iii).
Health by Socioeconomic Status
Ximena de la Barra, senior urban advisor to UNICEF, wrote in 1998 that "being poor is in itself a health hazard; worse, however, is being urban and poor" (de la Barra 1998 p. 46). The context of her statement was global urban poverty, but her conclusions apply to the relationship between poverty and health in Canada as well. Residents of poorer urban areas in Canada have significantly higher hospitalization rates and lower self-reported quality of health than residents of average or wealthy urban areas (see Figures 19.6 and 19.7). Living and growing up in poverty is linked to lower life expectancy, and chronic illnesses such as diabetes, mental illness, stroke, cardiovascular disease, central nervous system disease, and injury (Canadian Population Health Initiative 2008). In fact actual medical care accounts for only about a quarter of health outcomes, while one-half of a person's ability to recover from illness is determined by socioeconomic factors, including income, education, and living conditions (CBC 2014). In an interesting study of 17, 350 British civil servants, it was found that differences in even relatively small disparities of wealth and power between civil service employment grades led to significantly better health outcomes for the privileged. The more authority one has, the healthier one is (Marmot, Shipley, and Rose 1984). These social determinants of health led the Canadian Medical Association to argue that providing adequate financial resources might be the best medical treatment that can be provided to poor patients. Inner city doctor, Gary Bloch stated, "Treating people at low income with a higher income will have at least as big an impact on their health as any other drugs that I could prescribe them…. I do see poverty as a disease" (CBC 2013).
It is important to remember that economics are only part of the socioeconomic status (SES) picture; research suggests that education also plays an important role. Phelan and Link (2003) note that many behaviour-influenced diseases like lung cancer (from smoking), coronary artery disease (from poor eating and exercise habits), and AIDS initially were widespread across SES groups. However, once information linking habits to disease was disseminated, these diseases decreased in high SES groups and increased in low SES groups. This illustrates the important role of education initiatives regarding a given disease, as well as possible inequalities in how those initiatives effectively reach different SES groups.
Health by Gender
Women continue to live longer than men on average, but women have higher rates of disability and disease. In each age group, men have higher rates of fatal disease, whereas women have higher rates of non-fatal chronic disease. "Women get sicker but men die quicker" might be a way of summing this up (Lorber 2000). For example, while 4 percent of Canadian men suffer from chronic illnesses, these illnesses affect 11 percent of Canadian women, particularly conditions such as multiple sclerosis, lupus, migraines, hypothyroidism, and chronic pain (Spitzer 2005). While men's lower life expectancy is often attributed to three factors—their tendency to engage in riskier behaviour or riskier work than women, their lower use of the health care system (which prevents symptoms from being diagnosed earlier), and their innate biological disposition to higher mortality at every stage of life—it is not as clear why chronic disease affects women in higher proportions. Spitzer notes that gender roles and relations lead to different responses and exposures to stressors, different access to resources, different responsibilities with regard to domestic work and caregiving, and different levels of exposure to domestic violence, all of which affect chronic health issues in women disproportionately.
Women are also affected adversely by institutionalized sexism in health care provision. We can see an example of institutionalized sexism in the way that women are more likely than men to be diagnosed with certain kinds of mental disorders. Psychologist Dana Becker notes that 75 percent of all diagnoses of Borderline Personality Disorder (BPD) are for women according to the Diagnostic Statistical Manual of Mental Disorders . This diagnosis is characterized by instability of identity, of mood, and of behaviour, and Becker argues that it has been used as a catch-all diagnosis for too many women. She further decries the pejorative connotation of the diagnosis, saying that it predisposes many people, both within and outside of the profession of psychotherapy, against women who have been so diagnosed (Becker N.d.).
Many critics also point to the medicalization of women's issues as an example of institutionalized sexism. Medicalization refers to the process by which previously normal aspects of life are redefined as deviant and needing medical attention to remedy. Historically and contemporaneously, many aspects of women's lives have been medicalized, including menstruation, pre-menstrual syndrome, pregnancy, childbirth, and menopause. The medicalization of pregnancy and childbirth has been particularly contentious in recent decades, with many women opting against the medical process and choosing a more natural childbirth. Fox and Worts (1999) find that all women experience pain and anxiety during the birth process, but that social support relieves both as effectively as medical support. In other words, medical interventions are no more effective than social ones at helping with the difficulties of pain and childbirth. Fox and Worts further found that women with supportive partners ended up with less medical intervention and fewer cases of postpartum depression. Of course, access to quality birth care outside of the standard medical models may not be readily available to women of all social classes.
Making Connections: Sociology in the Real World
Medicalization of Sleeplessness
How is your "sleep hygiene?" Sleep hygiene refers to the lifestyle and sleep habits that contribute to sleeplessness or insomnia. Bad habits that can lead to sleeplessness include inconsistent bedtimes, lack of exercise, late-night employment, napping during the day, and sleep environments that include noise, lights, or screen time (National Institutes of Health 2011a).
According to the Toronto-based University Health Network, examining sleep hygiene is the first step in trying to solve a problem with sleeplessness (Bernstein and Durkee 2008).
For many North Americans, however, making changes in sleep hygiene does not seem to be enough. According to a 2006 report, sleeplessness is an underrecognized public health problem affecting up to 70 million people. It is interesting to note that in the months (or years) after this report was released, advertising by the pharmaceutical companies behind Ambien, Lunesta, and Sepracor (three sleep aids) averaged $188 million weekly promoting these drugs (Gellene 2009).
According to Moloney, Konrad, and Zimmer (2011), prescriptions for sleep medications increased dramatically from 1993 to 2007. While complaints of sleeplessness during doctor's office visits more than doubled during this time, insomnia diagnoses increased more than sevenfold, from about 840,000 to 6.1 million. The authors of the study conclude that sleeplessness has been medicalized as insomnia, and that "insomnia may be a public health concern, but potential overtreatment with marginally effective, expensive medications with nontrivial side effects raises definite population health concerns" (Moloney, Konrad, and Zimmer 2011). Indeed, a study published in 2004 in the Archives of Internal Medicine shows that cognitive behavioural therapy, not medication, was the most effective sleep intervention (Jacobs, Pace-Schott, Stickgold, and Otto 2004).
A century ago, people who couldn't sleep were told to count sheep. Now, they pop a pill, and all those pills add up to a very lucrative market for the pharmaceutical industry. Is this industry behind the medicalization of sleeplessness, or are they just responding to a need?
Mental Health and Disability
The treatment received by those defined as mentally ill or disabled varies greatly from country to country. In post-millennial Canada, those of us who have never experienced such a disadvantage take for granted the rights our society guarantees for each citizen. However, access to things like education, housing, or transportation that most people take for granted, are often experienced very differently by people with disabilities.
Mental Health
People with mental disorders (a condition that makes it more difficult to cope with everyday life) and people with mental illness (a severe, lasting mental disorder that requires long-term treatment) experience a wide range of effects.
According to the 2012 Canadian Community Health Survey, the most common mental disorders in Canada are mood disorders (major depression, bipolar disorder). Over 11 percent of Canadians reported experiencing major episodes of depression in their lifetime (4.7 percent in the previous year), while 2.6 percent reported bipolar disorder in their lifetime (1.5 percent in the previous year) (Pearson, Janz, and Ali 2013). Major mood disorders are depression, bipolar disorder, and dysthymic disorder. Depression might seem like something that everyone experiences at some point, and it is true that most people feel sad or "blue" at times in their lives. A true depressive episode, however, is more than just feeling sad for a short period. It is a long-term, debilitating illness that usually needs treatment to cure. Bipolar disorder is characterized by dramatic shifts in energy and mood, often affecting the individual's ability to carry out day-to-day tasks. Bipolar disorder used to be called manic depression because of the way that people would swing between manic and depressive episodes.
The second most common mental disorders in Canada are anxiety disorders. Almost 9 percent of Canadians reported experiencing generalized anxiety disorder in their lifetime (2.6 percent in the previous year) (Pearson, Janz, and Ali 2013). Similar to depression, it is important to distinguish between occasional feelings of anxiety and a true anxiety disorder. Anxiety is a normal reaction to stress that we all feel at some point, but anxiety disorders are feelings of worry and fearfulness that last for months at a time. Anxiety disorders include obsessive compulsive disorder (OCD), panic disorders, posttraumatic stress disorder (PTSD), and both social and specific phobias.
Depending on what definition is used, there is some overlap between mood disorders and personality disorders. Canadian data on the prevalence of personality disorders is lacking but estimates in the United States suggest they affect 9 percent of Americans yearly. In Canada, epidemiological research reporting on antisocial personality disorder shows that about 1.7 percent of the population experience this specific disorder yearly (Public Health Agency of Canada 2002). The American Psychological Association publishes the Diagnostic and Statistical Manual on Mental Disorders (DSM), and their definition of personality disorders is changing in the fifth edition, which is being revised in 2011 and 2012. In the DSM-IV, personality disorders represent "an enduring pattern of inner experience and behaviour that deviates markedly from the expectations of the culture of the individual who exhibits it" (National Institute of Mental Health). In other words, personality disorders cause people to behave in ways that are seen as abnormal to society but seem normal to them. The DSM-V proposes broadening this definition by offering five broad personality trait domains to describe personality disorders, some related to the level or type of their disconnect with society. As their application evolves, we will see how their definitions help scholars across disciplines understand the intersection of health issues and how they are defined by social institutions and cultural norms.
Another fairly commonly diagnosed mental disorder is attention-deficit/hyperactivity disorder (ADHD), which American statistics suggest affects 9 percent of children and 8 percent of adults on a lifetime basis (National Institute of Mental Health 2005). The New York Times reported American Centers for Disease Control data showing that the diagnosis of children with ADHD had increased by 53 percent over the last decade, raising issues of overdiagnosis and overmedication (Schwarz and Cohen 2013). Recent data from Canada confirm the increasing rate of prescribed medications and ADHD diagnosis in Canada, although the rates are much lower than those reported in the United States (3 percent for all children aged three to nine, but 4 percent for boys and 5 percent for school-aged children in this age range) (Brault and Lacourse 2012). ADHD is one of the most common childhood disorders, and it is marked by difficulty paying attention, difficulty controlling behaviour, and hyperactivity. The significant increase in diagnosis and the use of medications such as Ritalin have prompted social debate over whether such drugs are being overprescribed (American Psychological Association, N.d.). In fact, some critics question whether this disorder is really as widespread as it seems, or if it is a case of overdiagnosis.
Autism spectrum disorders (ASD) have also gained a lot of attention in recent years. The term ASD encompasses a group of developmental brain disorders that are characterized by "deficits in social interaction, verbal and nonverbal communication, and engagement in repetitive behaviours or interests" (National Institute of Mental Health, 2011b). A report from the American Centers for Disease Control (CDC) suggests that 1 in every 68 children is born with ASD (Centers for Disease Control and Prevention 2014). This diagnosis is up by 30 percent from the previous estimate that 1 in 88 children is born with ASD. In Canada, a national tracking system is being set up, but a report from the National Epidemiologic Database for the Study of Autism in Canada found increases in diagnosis in Prince Edward Island, Newfoundland and Labrador, and southeastern Ontario ranging from 39 to 204 percent, depending on the region. As an example of social construction of disorders, much of the increase in diagnosis is believed to be due to increased awareness of the disorder rather than actual prevalence, with doctors diagnosing autism more frequently and with children with less severe problems (NEDSAC 2012).
The National Institute of Mental Health (NIMH) distinguishes between serious mental illness and other disorders. The key feature of serious mental illness is that it results in "serious functional impairment, which substantially interferes with or limits one or more major life activities" (National Institute of Mental Health 2005). Thus, the characterization of "serious" refers to the effect of the illness (functional impairment), not the illness itself.
Although the view is not widely held, there are some researchers who argue that mental illness is a myth. For example, to Thomas Scheff (1963), residual deviance—a violation of social norms not covered by any specific behavioural expectation—is what actually results in people being labelled mentally ill. In The Myth of Mental Illness: Foundations of a Theory of Personal Conduct (1961), Thomas Szasz asks if there is such a thing as mental illness, and then argues that there is not. Rather, mental illness is a deviation from what others view as normal, with no basis in biological disease. Szasz calls for greater personal responsibility and less reliance on institutions.
Disability
Disability refers to a reduction in one's ability to perform everyday tasks. The World Health Organization makes a distinction between the various terms used to describe handicaps that's important to the sociological perspective. They use the term impairment to describe the physical limitations, while reserving the term disability to refer to the social limitation. In 2012, 3.8 million Canadians, or 13.7 percent of Canadians aged 15 and over, reported having a disability—a long-term condition or health-related problem—that limited their ability to perform daily tasks. Twenty-six percent of these disabled Canadians had a disability classified as "very severe" (Statistics Canada 2013).
Lyn Jongbloed (2003) notes that conceptions of disability have gone through several shifts in Canada since the 19th century, leading to significant shifts in public policy on disabilities. In the early 19th century, persons with intellectual impairments were often jailed alongside criminals, suggesting that the distinction was not significant from the point of view of public policy. Then between 1860 and 1890, the asylum model of care was developed specifically for the disabled, in large part to protect them or others from harm. People with physical disabilities were not regarded as disruptive so they were not institutionalized. This law and order approach was gradually replaced by medical and economic models that conceptualized disability as a biological reality that called for practices such asrehabilitation. Rehabilitation focused on interventions to treat or cure disabilities so that disabled persons could earn a livelihood and reintegrate into "normal" society. As Jongbloed suggests, "Helping people become economically independent is consistent with the North American ideology of individualism. The economic model of disability is predicated on an individual's inability to participate in the paid labour force" (2003, p. 205). Finally, since the 1970s, the medical and economic model has been gradually supplanted, or supplemented, by a sociopolitical model that argues that disability results from a failure of the social environment rather than individual impairment. This led to rights-based challenges of barriers to the disabled and a deinstutionalization movement that saw the closing of the asylum system and its replacement with a community model of care.
Before the passage of the Canadian Charter of Rights and Freedoms in 1982, which specifically designated individuals with disabilities as one of four disadvantaged groups protected by the Charter, Canadians with disabilities were often routinely excluded from opportunities and social institutions that many able-bodied persons take for granted. This occurred not only through employment and other kinds of discrimination, but through casual acceptance by most Canadians of a world designed for the convenience of the able-bodied. Imagine being in a wheelchair and trying to use a sidewalk without the benefit of wheelchair-accessible curbs. Imagine as a blind person trying to access information without the widespread availability of Braille. Imagine having limited motor control and being faced with a difficult-to-grasp round door handle.Ableism refers to both direct discrimination against persons with disabilities and the unintended neglect of their needs.
Ableism is linked to the enduring legacy of stigmatizing persons with disabilities. People with disabilities are stigmatized by the perception that they are, in some manner, ill.Stigmatization means that their identity is spoiled; they are labelled as different, discriminated against, and sometimes even shunned. They are labelled (as an interactionist might point out) and ascribed a master status (as a functionalist might note), becoming "the blind girl" or "the boy in the wheelchair" instead of someone afforded a full identity by society. This can be especially true for people who are disabled due to mental illness or disorders. In response, many disabled groups have begun to assert that they are not disabled, but differently enabled. Their condition is not a form of deviance from the norm, but a different form of normality. As Rod Michalko argues, blindness for example is only seen as a problem or disability from the point of view of sightedness and a world organized for the sighted (Michalko 1998).
As discussed in the section on mental health, many mental health disorders can be debilitating, affecting a person's ability to cope with everyday life. This can affect social status, housing, and especially employment. According to the a Canadian Human Rights Commission'sReport on Equity Rights of People with Disabilities (2012), people with a disability had a higher rate of unemployment than people without a disability: 8.6 percent to 6.3 percent (2006 data). Disabled men and women are also 8.6 percent and 6.5 percent more likely to be underemployed than men and women without disabilities (respectively). The disabled were also only half as likely to complete a university education than the non-disabled (20.2 per cent versus 40.7 per cent, respectively) and earned significantly less than they do ($9,557 less per year for men and $8,853 less for women).
Making Connections: Sociology in the Real World
Obesity: The Last Acceptable Prejudice
What is your reaction to the picture in Figure 19.9? Compassion? Fear? Disgust? Many people will look at this picture and make negative assumptions about the man based on his weight. According to a study from the Yale Rudd Center for Food Policy and Obesity, large people are the object of "widespread negative stereotypes that overweight and obese persons are lazy, unmotivated, lacking in self-discipline, less competent, noncompliant, and sloppy" (Puhl and Heuer 2009).
Historically, both in Canada and elsewhere, it was considered acceptable to discriminate against people based on prejudiced opinions. Even after colonization formally ended with the formation of the Canadian state in 1867, the next 100 years of Canadian history saw institutionalized racism and prejudice against aboriginal people. In an example of stereotype interchangeability, the same insults that are flung today at the overweight and obese population (lazy, for instance), have been flung at various racial and ethnic groups in earlier history. Of course, no one gives voice to these kinds of views in public now, except when talking about obese people.
Why is it considered acceptable to feel prejudice toward—even to hate—obese people? Puhl and Heuer suggest that these feelings stem from the perception that obesity is preventable through self-control, better diet, and more exercise. Highlighting this contention is the fact that studies have shown that people's perceptions of obesity are more positive when they think the obesity was caused by non-controllable factors like biology (a thyroid condition, for instance) or genetics.
Even with some understanding of non-controllable factors that might affect obesity, obese people are still subject to stigmatization. Puhl and Heuer's study is one of many that document discrimination at work, in the media, and even in the medical profession. Obese people are less likely to get into college than thinner people, and they are less likely to succeed at work.
Stigmatization of obese people comes in many forms, from the seemingly benign to the potentially illegal. In movies and television shows, overweight people are often portrayed negatively, or as stock characters who are the butt of jokes. One study found that in children's movies "obesity was equated with negative traits (evil, unattractive, unfriendly, cruel) in 64 percent of the most popular children's videos. In 72 percent of the videos, characters with thin bodies had desirable traits, such as kindness or happiness" (Hines and Thompson 2007). In movies and television for adults, the negative portrayal is often meant to be funny. "Fat suits"—inflatable suits that make people look obese—are commonly used in a way that perpetuates negative stereotypes. Think about the way you have seen obese people portrayed in movies and on television; now think of any other subordinate group being openly denigrated in such a way. It is difficult to find a parallel example.
19.4. Theoretical Perspectives on Health and Medicine
Each of the three major theoretical perspectives approaches the topics of health, illness, and medicine differently.
Functionalism
According to the functionalist perspective, health is vital to the stability of the society, and therefore sickness is a sanctioned form of deviance. Talcott Parsons (1951) was the first to discuss this in terms of the sick role: patterns of expectations that define appropriate behaviour for the sick and for those who take care of them.
According to Parsons, the sick person has a specific role with both rights and responsibilities. To start with, in the context of modern norms of individualism and individual responsibility, a person has not chosen to be sick and should not be treated as responsible for his or her condition. The sick person also has the right of being exempt from normal social roles; the person is not required to fulfill the obligation of a well person and can avoid normal responsibilities without censure. However, this exemption is temporary and relative to the severity of the illness. The exemption also requires legitimation by a physician; that is, a physician must certify that the illness is genuine.
The responsibility of the sick person is twofold: to try to get well and to seek technically competent help from a physician. If the sick person stays ill longer than is appropriate (malingers), he or she may be stigmatized.
Parsons argues that since the sick are unable to fulfill their normal societal roles, their sickness weakens the society. Therefore, it is sometimes necessary for various forms of social control to bring the behaviour of a sick person back in line with normal expectations. In this model of health, doctors serve as gatekeepers, deciding who is healthy and who is sick—a relationship in which the doctor has all the power. But is it appropriate to allow doctors so much power over deciding who is sick? And what about people who are sick, but are unwilling to leave their positions for any number of reasons (personal/social obligations, financial need, or lack of insurance, for instance).
Critical Sociology
Theorists using the critical perspective suggest that many issues with the health care system, as with most other social problems, are rooted in capitalist society. According to critical sociology, capitalism and the pursuit of profit lead to the commodification of health: the changing of something not generally thought of as a commodity into something that can be bought and sold in a marketplace. In this view, corporations, private insurance companies, pharmaceutical companies and investors have a disproportionate influence over how the health care system is run and funded, which type of diseases are researched, whether cheaper generic versions of patented drugs can be sold, the nature of the health care delivered, and even how the physiology of the human body is understood. Corporate interests also influence the terms in which debates about public health care are discussed. Corporate think tanks like the Fraser Institute and the CD Howe Institute have long advocated free-market, profit-driven, American-style models rather than publicly funded models to deliver health care in Canada (Carroll and Shaw 2001). The language with which they approach health care emphasizes "taxpayer rights," alarming statements about the financial unsustainability of public health care, and the role of "vested interests" in promoting an outdated 1960s-era system. Despite the fact that Canadians persistently state that public, universal health care is their central priority, corporate and neoliberal messaging on health care has become increasingly influential over the last two decades.
Alongside the health disparities created by class inequalities, there are a number of health disparities created by racism, sexism, ageism, and heterosexism. When health is a commodity, the poor are more likely to experience illness caused by poor diet, to live and work in unhealthy environments, and are less likely to challenge the system. In Canada, aboriginal people have been disproportionately marginalized from economic power, so they bear a great deal of the burden of poor health.
Another critical approach to health and illness focuses on the emergence of biopolitics in the 18th and 19th centuries (Foucault 1980). Biopolitics refers to the relationships of power that emerge when the task of fostering and administering the "life" of the population becomes central to government (in the broad sense of the term: see Chapter 17). In a variety of different levels and sites in society—from implementing society-wide public health programs and population controls to various forms of discipline exercised over the bodies of patients, soldiers, children, students, and prisoners—modern scientific knowledge on the functioning of the body establishes new power relations between experts (e.g., doctors, psychiatrists, psychologists, sociologists, social workers) and subjects. As a result, increasingly numerous forms of discipline and regulation emerge that seek to act upon the living body and the living population to maximize their potential for health, productivity, efficiency, and docility.
Modern biomedicine, for example, is a system of medical practice that defines health and illness in terms of the mechanics of the physical, biological systems of the human body. It works on the basis of a mind/body division that leads the individual to "inhabit" his or her body and its problems in a certain way and to submit, voluntarily or involuntarily, to the expertise of doctors when bodily function deviates from biological norms. It is on the basis of doctors' claim to biomedical knowledge that individuals submit to more or less mortifying exercises of power and discipline: from dieting and exercise regimes to pharmaceutical drug treatments to caesarian births to chemotherapy and gene therapy.
It is interesting in this respect to note the various ways in which the knowledge and authority of doctors and the medical establishment are being challenged in contemporary society. People are increasingly researching and becoming more knowledgeable about their health concerns in a manner that permits them to engage with doctors and medical authorities on a more equal basis. They are also engaging with an expanding range of alternatives to conventional biomedicine: health practices and knowledge such as yoga, fitness regimes, dieting, acupuncture, traditional Chinese medicine, chi gong, naturopathy, homeopathy, chiropractic, and indigenous healing practices. This turn to a model of individualized care for the self—i.e., ways of acting upon the self to transform the self to attain a certain mode of being such as "health" (Foucault 1997)—has a number of competing implications, however. On the one hand, it enables practices of autonomy and self-formation freed from the power relations of the medical establishment. On the other hand, it can feed into intensified concerns and anxieties with the body that deepen rather than loosen submission to authorities and authoritative knowledge—dieting fads, esoteric knowledge and practices, and nontraditional healers, etc. As Zygmunt Bauman notes, when individuals take on the responsibility for knowledge about their own bodies and health in a pluralistic medical culture in which there are numerous competing and contradicting claims about treatment, the outcome for the individual can be paralyzing rather than liberating (Bauman 2005).
Symbolic Interactionism
According to theorists working in this perspective, health and illness are both socially constructed. As we discussed in the beginning of the chapter, interactionists focus on the specific meanings and causes people attribute to illness. The term medicalization of deviance refers to the process that changes "bad" behaviour into "sick" behaviour. A related process is demedicalization, in which "sick" behaviour is normalized again. Medicalization and demedicalization affect who responds to the patient, how people respond to the patient, and how people view the personal responsibility of the patient (Conrad and Schneider 1992).
An example of medicalization is illustrated by the history of how our society views alcohol and alcoholism. During the 19th century, people who drank too much were considered bad, lazy people. They were called drunks, and it was not uncommon for them to be arrested or run out of a town. Drunks were not treated in a sympathetic way because, at that time, it was thought that it was their own fault that they could not stop drinking. By the late 19th century however, excessive drinking became regarded as a "disease of the will"—a paradoxical illness that required the patient to actively engage in his or her own treatment, even though the nature of the disease was defined by a defect in the will that undermined his or her ability to do so (Valverde 1997). In the 20th century, people who drank too much were increasingly defined as alcoholics: people with a psychological dependence, physiological disease, or a genetic predisposition to addiction who were not responsible for their drinking. With alcoholism defined as a disease and not a personal choice, alcoholics came to be viewed with more compassion and understanding, although the paradox of recovery therapies for alcoholics remained. Thus, "badness" was transformed into "sickness."
There are numerous examples of demedicalization in history as well. During the Civil War era, slaves who frequently ran away from their owners were diagnosed with a mental disorder called drapetomania. This has since been reinterpreted as a completely appropriate response to being enslaved. A more recent example is homosexuality, which was labelled a mental disorder or a sexual orientation disturbance by the American Psychological Association until 1973.
While interactionism does acknowledge the subjective nature of diagnosis, it is important to remember who most benefits when a behaviour becomes defined as illness. Pharmaceutical companies make billions treating illnesses such as fatigue, insomnia, and hyperactivity that may not actually be illnesses in need of treatment, but opportunities for companies to make more money.
Key Terms
ableism discrimination against persons with disabilities or the unintended neglect of their needs
anxiety disorders feelings of worry and fearfulness that last for months at a time
biomedicine a system of medical practice that defines health and illness in terms of the mechanics of the physical, biological systems of the human body
biopolitics the relationships of power that emerge when the task of fostering and administering the life of the population becomes central to government
care for the self ways of acting upon the self to transform the self to attain a certain mode of being (e.g., "health")
commodification the changing of something not generally thought of as a commodity into something that can be bought and sold in a marketplace
contested illnesses illnesses that are questioned or considered questionable by some medical professionals
demedicalization the social process that normalizes "sick" behavior
disability a reduction in one's ability to perform everyday tasks; the World Health Organization notes that this is a social limitation
health a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity
impairment the physical limitations a less-able person faces
legitimation when a physician certifies that an illness is genuine
medical sociology the systematic study of how humans manage issues of health and illness, disease and disorders, and health care for both the sick and the healthy
medicalization the process by which aspects of life that were considered bad or deviant are redefined as sickness and needing medical attention to remedy
medicalization of deviance the process that changes "bad" behaviour into "sick" behavior
mood disorders long-term, debilitating illnesses like depression and bipolar disorder
personality disorders disorders that cause people to behave in ways that are seen as abnormal to society but seem normal to them
public health care health insurance that is funded or provided by the government
sick role the pattern of expectations that define appropriate behaviour for the sick and for those who take care of them
rehabilitation interventions to treat or cure disabilities in order to reintegrate disabled persons into "normal" society
social epidemiology the study of the causes and distribution of diseases
stereotype interchangeability when stereotypes don't change, they get recycled for application to a new subordinate group
stigmatization when someone's identity is spoiled; they are labelled as different, discriminated against, and sometimes even shunned due to an illness or disability
stigmatization of illness when people are discriminated against because of illnesses and sufferers are looked down upon or even shunned by society
universal health care a system that guarantees health care coverage for everyone
Section Summary
19.1. The Social Construction of Health
Medical sociology is the systematic study of how humans manage issues of health and illness, disease and disorders, and health care for both the sick and the healthy. The social construction of health explains how society shapes and is shaped by medical ideas.
19.2. Global Health
Social epidemiology is the study of the causes and distribution of diseases. From a global perspective, the health issues of high-income nations tend toward diseases like cancer as well as those that are linked to obesity, like heart disease, diabetes, and musculoskeletal disorders. Low-income nations are more likely to contend with infectious disease, high infant mortality rates, scarce medical personnel, and inadequate water and sanitation systems.
19.3. Health in Canada
Despite the Canadian population having generally good health compared with less-developed countries, Canada is still facing challenging issues such as a prevalence of obesity and diabetes. Moreover, Canadians of historically disadvantaged aboriginal groups, socioeconomic status, and gender experience higher levels of chronic health issues. Mental health and disability are health issues that are significantly impacted by medical definitions of normalcy.
19.4 Theoretical Perspectives on Health and Medicine
While the functionalist perspective looks at how health and illness define specific roles in society, the critical perspective is concerned with how health and illness fit into the structures of power in society. The interactionist perspective is concerned with how social interactions construct ideas of health and illness.
Section Quiz
19.1. The Social Construction of Health
1. Who determines which illnesses are stigmatized?
- Therapists
- The patients themselves
- Society
- All of the above
2. Chronic fatigue syndrome is an example of _______________.
- A stigmatized disease
- A contested illness
- A disability
- Demedicalization
3. The Rating of Perceived Exertion (RPE) is an example of ________________
- The social construction of health
- Medicalization
- Disability accommodations
- A contested illness
19.2. Global Health
4. What is social epidemiology?
- The study of why some diseases are stigmatized and others are not
- The study of why diseases spread
- The study of the mental health of a society
- The study of the causes and distribution of diseases
5. Core nations are also known as __________________
- High-income nations
- Newly industrialized nations
- Low-income nations
- Developing nations
6. Many deaths in high-income nations are linked to __________________
- Lung cancer
- Obesity
- Mental illness
- Lack of clean water
7. According to the World Health Organization, what was the most frequent cause of death for children under five in low-income countries?
- Starvation
- Thirst
- Pneumonia and diarrheal diseases
- All of the above
19.3. Health in Canada
8. Which of the following statements is not true?
- The life expectancy of aboriginal males in the Canada is approximately eight years shorter than for non-aboriginal males.
- The rate of tuberculosis for aboriginal Canadians is more than five times higher (per 100,000) than it is for non-aboriginal Canadians.
- Aboriginal people have lower rates of chronic disease than non-aboriginal people.
- Recent visible minority immigrants have lower levels of health than native-born Canadians.
9. The process by which aspects of life that were considered bad or deviant are redefined as sickness and needing medical attention to remedy is called ___________.
- Deviance
- Medicalization
- Demedicalization
- Intersection theory
10. What are the most commonly diagnosed mental disorders in Canada?
- ADHD
- Anxiety disorders
- Autism spectrum disorders
- Mood disorders
11. Sidewalk ramps and Braille signs are examples of _______________.
- Disabilities
- Accommodations required by the Canadian Charter of Rights and Freedoms
- Forms of accessibility for people with disabilities
- Both b and c
12. The high unemployment rate among the disabled may be a result of ____________.
- Medicalization
- Obesity
- Stigmatization
- All of the above
19.4. Theoretical Perspectives on Health and Medicine
13. Which of the following is not part of the rights and responsibilities of a sick person under the functionalist perspective?
- The sick person is not responsible for his or hercondition.
- The sick person must try to get better.
- The sick person can take as long as he or she wants to get better.
- The sick person is exempt from the normal duties of society.
14. The class, race, and gender inequalities in our healthcare system support the _____________ perspective.
- Critical
- Interactionist
- Functionalist
- All of the above
15. The removal of homosexuality from the DSM is an example of ____________.
- Medicalization
- Deviance
- Interactionist theory
- Demedicalization
Short Answer
19.1. The Social Construction of Health
- Pick a common illness and describe which parts of it are medically constructed, and which parts are socially constructed.
- What diseases are the most stigmatized? Which are the least? Is this different in different cultures or social classes?
19.2. Global Health
- If social epidemiologists studied Canada in the colonial period, what differences would they find between now and then?
- What do you think are some of the contributing factors to obesity-related diseases in Canada?
19.3. Health in Canada
- What factors contribute to the disparities in health among ethnic, socioeconomic, and gender groups in Canada?
- Do you know anyone with a mental disorder? How does it affect his or her life?
19.4. Theoretical Perspectives on Health and Medicine
- Which theoretical perspective do you think best explains the sociology of health? Why?
- What examples of medicalization and demedicalization can you think of?
Further Research
19.1. The Social Construction of Health
Spend some time on the two websites below. How do they present differing views of the vaccination controversy? Freedom of Choice is Not Free: Vaccination News: http://openstaxcollege.org/l/vaccination_news and Shot by Shot: Stories of Vaccine-Preventable Illnesses: http://openstaxcollege.org/l/shot_by_shot
19.2. Global Health
Study this map on global life expectancies: http://openstaxcollege.org/l/global_life_expectancies. What trends do you notice?
19.3. Health in Canada
Is ADHD a valid diagnosis and disease? Some think it is not. This article discusses ADHD: http://www.mentalhealthcanada.com/ConditionsandDisordersDetail.asp?lang=e&category=60
19.4. Theoretical Perspectives on Health and Medicine
Should alcoholism and other addictions be medicalized? Read and watch a dissenting view: http://openstaxcollege.org/l/addiction_medicalization
References
19.. Introduction to Health and Medicine
Centers for Disease Control. 2011."Pertussis." The Centers for Disease Control and Prevention. Retrieved December 15, 2011 (http://www.cdc.gov/pertussis/outbreaks.html).
CNN. 2011. "Retracted Autism Study an 'Elaborate Fraud,' British Journal Finds." CNN, January 5. Retrieved December 16, 2011 (http://www.cnn.com/2011/HEALTH/01/05/autism.vaccines/index.html).
Devlin, Kate. 2008. "Measles worry MMR as vaccination rates stall." The Telegraph, September 24. Retrieved January 19, 2012 (http://www.telegraph.co.uk/news/uknews/3074023/Measles-worries-as-MMR-vaccination-rates-stall.html).
Picard, André. 2012. "Comeback of a deadly disease, and where we went wrong." Toronto Globe and Mail. July 23. Retrieved July 27, 2014, from http://www.theglobeandmail.com/life/health-and-fitness/health/comeback-of-a-deadly-disease-and-where-we-went-wrong/article4436993/
Sugerman, David E., Albert E. Barskey, Maryann G. Delea, Ismael R. Ortega-Sanchez, Daoling Bi, Kimberly J. Ralston, Paul A. Rota, Karen Waters-Montijo, and Charles W. LeBaron. 2010. "Measles Outbreak in a Highly Vaccinated Population, San Diego, 2008: Role of the Intentionally Undervaccinated." Pediatrics 125(4):747–755. Retrieved December 16, 2011 (http://www.pediatricsdigest.mobi/content/125/4/747.full).
WHO 2014. "What Is the WHO Definition of Health?(Frequently Asked Questions)" World Health Organization. Retrieved July 28, 2014, from http://www.who.int/suggestions/faq/en/
Zacharyczuk, Colleen. 2011. "Myriad causes contributed to California pertussis outbreak." Thorofar, NJ: Pediatric Supersite. Retrieved December 16, 2011 (http://www.pediatricsupersite.com/view.aspx?rid=90516).
19.1. The Social Construction of Health
Begos, Kevin. 2011. "Pinkwashing For Breast Cancer Awareness Questioned." Huffington Post. Retrieved December 16, 2011 (http://www.huffingtonpost.com/2011/10/11/breast-cancer-pink-pinkwashing_n_1005906.html).
Conrad, Peter and Kristin Barker. 2010. "The Social Construction of Illness: Key Insights and Policy Implications." Journal of Health and Social Behavior 51:67–79.
CSEP. n.d. "PAL Physical Activity Line: Rating of Perceived Exertion scale." Canadian Society for Exercise Physiology. Retrieved July 27, 2014, from http://www.physicalactivityline.com/pdf_files/pal-doc-perceivedexertionscale.pdf
Goffman, Erving. 1963. Stigma: Notes on the Management of Spoiled Identity. London: Penguin.
Hutchison, Courtney. 2010. "Fried Chicken for the Cure?" ABC News Medical Unit. Retrieved December 16, 2011 (http://abcnews.go.com/Health/Wellness/kfc-fights-breast-cancer-fried-chicken/story?id=10458830#.Tutz63ryT4s).
Sartorius, Norman. 2007. "Stigmatized Illness and Health Care." The Croatian Medical Journal 48(3):396–397. Retrieved December 12, 2011 (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2080544/).
Think Before You Pink. 2012. "Before You Buy Pink." Retrieved December 16, 2011 (http://thinkbeforeyoupink.org/?page_id=13).
19.2. Global Health
Bromet et al. 2011. "Cross-National Epidemiology of DSM-IV Major Depressive Episode." BMC Medicine 9:90. Retrieved December 12, 2011 (http://www.biomedcentral.com/1741-7015/9/90).
Huffman, Wallace E., Sonya Kostova Huffman, AbebayehuTegene, and KyrreRickertsen. 2006. "The Economics of Obesity-Related Mortality among High Income Countries" International Association of Agricultural Economists. Retrieved December 12, 2011 (http://purl.umn.edu/25567).
Organisation for Economic Co-operation and Development. 2013. Health at a Glance 2013: OECD Indicators. OECD Publishing. Retrieved July 27, 2014, from http://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance_19991312;jsessionid=11239ofxudi0c.x-oecd-live-01
UNICEF. 2011. "Water, Sanitation and Hygiene." Retrieved December 12, 2011 (http://www.unicef.org/wash).
World Health Organization. 2011. "World Health Statistics 2011." Retrieved December 12, 2011 (http://www.who.int/gho/publications/world_health_statistics/EN_WHS2011_Part1.pdf).
19.3. Health in Canada
American Psychological Association. N.d. "Understanding the Ritalin Debate." American Psychological Association. Retrieved December 14, 2011 (http://www.apa.org/topics/adhd/ritalin-debate.aspx)
Becker, Dana. N.d. "Borderline Personality Disorder: The Disparagement of Women through Diagnosis." Retrieved December 13, 2011 (http://www.awpsych.org/index.php?option=com_content&view=article&id=109&catid=74&Itemid=126).
Bernstein, Lori and Linda Durkee. 2008. "Sleep Hygiene: Helpful Hints for Better Sleeping." University Health Network. October. Retrieved July 27, 2014, from http://www.uhn.ca/docs/HealthInfo/Shared%20Documents/Sleep_Hygiene_Helpful_Hints_to_Make_You_Sleep_Better.pdf
Brault, MC and É Lacourse. 2012. "Prevalence of prescribed attention-deficit hyperactivity disorder medications and diagnosis among Canadian preschoolers and school-age children: 1994-2007." Canadian Journal of Psychiatry. Feb. 57(2): 93-101.
Canadian Human Rights Commission. 2012. Report on Equality Rights of People with Disabilities. Minister of Public Works and Government Services. Catalogue no. HR4-20/2012E-PD. Retrieved July 30, 2014, from http://www.chrc-ccdp.ca/sites/default/files/rerpd_rdepad-eng.pdf
Canadian Population Health Initiative. 2008. Reducing Gaps in Health: A Focus on Socio-Economic Status in Urban Canada. Ottawa: Canadian Institute for Health Information. Retrieved July 29, 2014, from https://secure.cihi.ca/free_products/Reducing_Gaps_in_Health_Report_EN_081009.pdf
CBC. 2013. "Treating poverty works like medicine, doctors say: Financial support can pay off with better health" CBC News. May 26. Retrieved July 29, 2014, from http://www.cbc.ca/news/health/treating-poverty-works-like-medicine-doctors-say-1.1365662
CBC. 2014. "Project Money: Health and Wealth."The Current.July 15. Retrieved July 29, 2014, from http://www.cbc.ca/thecurrent/project-money/2014/07/15/health-and-wealth/
Centers for Disease Control and Prevention. 2014, March 28. "Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2010." MMWR. 63(2): 1-21. Retrieved August 2014, from http://www.cdc.gov/mmwr/pdf/ss/ss6302.pdf
de la Barra, Ximena 1998 "Poverty: The Main Cause of Ill Health in Urban Children," Health Education & Behavior 25, 1: 46-59
Fox, B. and D. Worts. 1999. "Revisiting the Critique of Medicalized Childbirth: A Contribution to the Sociology of Birth." Gender and Society 13(3):326–346.
Garner, Rochelle, Gisèle Carrière, Claudia Sanmartin. 2010. "The Health of First Nations Living Off -Reserve, Inuit, and Métis Adults in Canada: The Impact of Socio-economic Status on Inequalities in Health." Statistics Canada Catalogue no. 82-622-X No. 004. June. Retrieved July 28, 2014, from http://www.statcan.gc.ca/pub/82-622-x/82-622-x2010004-eng.pdf
Gellene, Denise. 2009. "Sleeping Pill Use Grows as Economy Keeps People up at Night." Retrieved December 16, 2011 (http://articles.latimes.com/2009/mar/30/health/he-sleep30).
Health Canada. 2005. "First Nations Comparable Health Indicators." First Nations and Inuit Health. Retieved July 28, 2014, from http://www.hc-sc.gc.ca/fniah-spnia/diseases-maladies/2005-01_health-sante_indicat-eng.php#life_expect
Hines, Susan M. and Kevin J. Thompson. 2007. "Fat Stigmatization in Television Shows and Movies: A Content Analysis." Obesity 15:712–718. Retrieved December 15, 2011 (http://onlinelibrary.wiley.com/doi/10.1038/oby.2007.635/full).
Jacobs, Gregg D., Edward F. Pace-Schott, Robert Stickgold, and Michael W. Otto. 2004. "Cognitive Behavior Therapy and Pharmacotherapy for Insomnia: A Randomized Controlled Trial and Direct Comparison." Archives of Internal Medicine 164(17):1888–1896. Retrieved December 16, 2011 (http://archinte.jamanetwork.com/article.aspx?articleid=217394 ).
Jongbloed, L. 2003. "Disability Policy in Canada: An Overview." Journal of Disability Policy Studies. 13(4): 203-209.
Kobayashi, Karen, Steven Prus, and Zhiqiu Lin. 2008. "Ethnic differences in selfrated and functional health: does immigrant status matter?" Ethnicity & Health. 13(2): 129-147
Lorber, Judith. 2000. "Women Get Sicker, but Men Die Quicker: Gender and Health" Pp. 40-70 in Phil Brown (ed.). Perspectives in Medical Sociology. Prospect Heights, Illinois: Waveland Press
Marmot, M.G., M.J. Shipley and G. Rose 1984 "Inequalities in Death—Specific Explanations of a General Pattern?" Lancet 1, 8384: 1003–1006.
Michalko, Rod. 1998. The Mystery of the Eye and the Shadow of Blindness. Toronto: University of Toronto Press.
Moloney, Mairead Eastin, Thomas R. Konrad, and Catherine R. Zimmer. 2011. "The Medicalization of Sleeplessness: A Public Health Concern." American Journal of Public Health 101:1429–1433.
National Institute of Mental Health. 2005. "National Institute of Mental Health Statistics." Retrieved December 14, 2011 (http://www.nimh.nih.gov/statistics/index.shtml).
National Institutes of Health. 2011a. "Insomnia." The National Institute of Health. Retrieved December 16, 2011 (http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001808/).
National Institutes of Health. 2011b. "What is Autism Spectrum Disorder (ASD)?" National Institute of Mental Health. Retrieved December 14, 2011 (http://www.nimh.nih.gov/health/publications/a-parents-guide-to-autism-spectrum-disorder/what-is-autism-spectrum-disorder-asd.shtml).
NEDSAC. 2012. "Findings from the National Epidemiologic Database for the Study of Autism in Canada (NEDSAC): Changes in the Prevalence of Autism Spectrum Disorders in Newfoundland and Labrador, Prince Edward Island, and Southeastern Ontario." National Epidemiologic Database for the Study of Autism in Canada. March. Retrieved September 25, 2014, from http://www.autismsocietycanada.ca/DocsAndMedia/KeyReports/NEDSAC_Report_March2012.pdf
O'Donnell, C. Vivien. 2008. "Native Populations in Canada."Pp. 285-293 in Garrick Bailey and William C. Sturtevant (ed.s). Handbook of North American Indians: Indians in Contemporary Society. Smithsonian Institute: Government Printing Office.
Pearson, Caryn, Teresa Janz and Jennifer Ali. 2013. "Mental and substance use disorders in Canada" Health at a Glance. Statistics Canada Catalogue no. 82-624-X. September. Retrieved July 27, 2014, from http://www.statcan.gc.ca/pub/82-624-x/2013001/article/11855-eng.htm
Phelan, Jo C. and Bruce G. Link. 2001. "Conceptualizing Stigma" Annual Review of Sociology 27:363–85. Retrieved December 13, 2011 (http://www.heart-intl.net/HEART/Legal/Comp/ConceptualizingStigma.pdf).
Phelan, Jo C. and Bruce G. Link. 2003. "When Income Affects Outcome: Socioeconomic Status and Health." Research in Profile:6. Retrieved December 13, 2011 (http://www.investigatorawards.org/downloads/research_in_profiles_iss06_feb2003.pdf).
Public Health Agency of Canada. 2002. "A Report on Mental Illnesses in Canada." Public Health Agency of Canada. Oct. 3. Retrieved July 27, 2014, from http://www.phac-aspc.gc.ca/publicat/miic-mmac/chap_5-eng.php
Puhl, Rebecca M. and Chelsea A. Heuer. 2009. "The Stigma of Obesity: A Review and Update." Nature Publishing Group. Retrieved December 15, 2011 (http://www.yaleruddcenter.org/resources/upload/docs/what/bias/WeightBiasStudy.pdf).
Scheff, Thomas. 1963. Being Mentally Ill: A Sociological Theory. Chicago, IL: Aldine.
Schwarz, Alan and Sarah Cohen. 2013. "A.D.H.D. Seen in 11% of U.S. Children as Diagnoses Rise." New York Times. March 31. Retrieved July 27, 2014, from http://www.nytimes.com/2013/04/01/health/more-diagnoses-of-hyperactivity-causing-concern.html?pagewanted=all&_r=0
Spitzer, Denise. 2005. "Engendering Health Disparities."Canadian Journal of Public Health. 96 (Supplement 2): 78- 96
Stastna, Kazi. 2011. "Clean running water still a luxury on many native reserves: About 39% of First Nations water systems deemed 'high risk'" CBC News. Nov 30. Retrieved July 28, 2014, from http://www.cbc.ca/news/canada/clean-running-water-still-a-luxury-on-many-native-reserves-1.1081705
Statistics Canada. 2011. "Aboriginal health and well-being" Canada Yearbook, Catalogue no.11-402-X. Retrieved July 28, 2014, from http://www41.statcan.gc.ca/2007/10000/ceb10000_004-eng.htm
Statistics Canada. 2013. "Canadian Survey on Disability, 2012." The Daily. Dec. 3. Retrieved July 30, 2014, from http://www.statcan.gc.ca/daily-quotidien/131203/dq131203a-eng.htm
Szasz, Thomas. 1961. The Myth of Mental Illness: Foundations of a Theory of Personal Conduct. New York, NY: Harper Collins.
Winkleby, Marilyn A., D. E. Jatulis, E. Frank, and S. P. Fortmann. 1992. "Socioeconomic Status and Health: How Education, Income, and Occupation Contribute to Risk Factors for Cardiovascular Disease." American Journal of Public Health 82:6.
W.H.O. 2014. "What Is the WHO Definition of Health?(Frequently Asked Questions)" World Health Organization. Retrieved July 28, 2014, from http://www.who.int/suggestions/faq/en/
19.4. Theoretical Perspectives on Health and Medicine
Bauman, Zygmunt. 2005. Liquid Life. Cambridge UK: Polity Press.
Carroll, William and Murray Shaw. 2001. "Consolidating a Neoliberal Policy Bloc in Canada, 1976 to 1996." Canadian Public Policy. 27(2): 195-217.
Conrad, Peter and Joseph W. Schneider. 1992. Deviance and Medicalization: From Badness to Sickness. Philadelphia, PA: Temple University Press.
Foucault, Michel. 1980. The History of Sexuality: Volume One. NY: Vintage Books.
Foucault, Michel. 1997. "The Ethics of the Concern of the Self as a Practice of Freedom." Pp. 281-302 in Paul Rabinow (ed.) Ethics: Subjectivity and Truth. NY: New York Press.
Parsons, Talcott. 1951. The Social System. Glencoe, IL: Free Press. Scheff, Thomas. 1963. "The Role of the Mentally Ill and the Dynamics of Mental Disorder." Sociometry 26:436–453.
Valverde, Mariana. 1997. "'Slavery from within': The Invention of Alcoholism and the Question of Free Will." Social History. 22(3): 251-268
Solutions to Section Quiz
1. C | 2. B | 3. A | 4. D | 5. A | 6. B | 7. C | 8. C | 9. B | 10. D | 11. D | 12. C | 13. C | 14. A | 15. D
America a Narrative History 10th Edition Chapter 20 Quizlet
Source: https://opentextbc.ca/introductiontosociology/chapter/chapter19-health-and-medicine/